This information note has been developed by the Eurasian Harm Reduction Network (EHRN) and the Eurasian Coalition on Male Health (ECOM) within the Global Fund's Community, Rights, and Gender (CRG) technical assistance program. It is intended for community-based organizations (CBOs), patient organizations, civil society organizations (CSOs), and groups working on HIV/AIDS and tuberculosis (TB) and with key affected populations (KAPs).
This information note is based on interviews with key stakeholders and parties involved in the development of the transition plan. The document provides recommendations for CBOs and CSOs to effectively influence the formation, implementation, and monitoring of the national HIV/AIDS and TB response in Georgia.
The purpose of this information note is to introduce the Transition and Sustainability Plan (TSP), which explains to the relevant organizations the process of transitioning the national HIV and TB response from Global Fund to domestic funding, and to emphasize the activities where the participation of CBOs and CSOs can play a crucial role. This information note presents activities from the TSP that are highly important for KAPs; it also provides information about the implementation timeline, responsible parties, monitoring indicators, and the budget. This document summarizes information in the TSP in a more user-friendly format to help communities and CSOs better understand their roles in the implementation of the plan. The TSP contains 55 activities, but for the purpose of this document only 28 of them have been selected, and the detailed tables about those activities are presented in the annex.
The information note also highlights the challenges related to the scale and sustainability of HIV and TB services intended for KAP under state funding. The UNAIDS 90–90–90 targets cannot be achieved without the active involvement of communities. Therefore, the title of this information note is based on the slogan "Nothing About Us Without Us".
Introduction
Georgia faces significant challenges with regard to HIV and TB prevalence. Stigma, discrimination, criminalization (among drug users), lack of peer-driven interventions, the medicalization of services, difficulties with contracting non-governmental organizations (NGOs) by the government, and many other factors represent barriers for the participation of patients and KAPs. The involvement of KAPs in the formation of the national HIV and TB response is particularly important during the transition of funding for those services to domestic sources, as this process defines whether current services will be maintained and improved, introduced and implemented at the community level, and thus provide an effective response to the epidemics.
A situational analysis of the TSP mentions that an increase in HIV and TB funding in Georgia was marginally targeted by the EU–Georgia Association Agreement in 2014. Specifically, pursuant to Article 356 of the agreement, Georgia shall strengthen "epidemiological surveillance and control of communicable diseases, such as for example HIV/AIDS, viral hepatitis, tuberculosis as well as antimicrobial resistance, as well as increased preparedness for public health threats and emergencies".
This aspect of Georgia’s obligations was included in the EU–Georgia Association Agreement to limit the number of individuals (representatives of KAPs) requesting asylum and treatment in European Union countries.
HIV/AIDS
HIV prevalence in the general population is low in Georgia, although incidence increases each year. Injecting drug use used to be the major mode of transmission; however, over recent years the prevailing mode of transmission has been heterosexual contact (see Figure 1). This can be explained mainly by transmission to sexual partners of people who inject drugs (PWID). Evidence suggests that the number of new cases has significantly increased among men who have sex with men (MSM). HIV prevalence among MSM doubles every three or four years; according to 2015 data, it had increased to 25.1% among this group (see Figure 2).
There are approximately 9600 HIV-positive people in Georgia, although half of them (49%) do not know their status. According to 2015 data, 70% of diagnosed HIV-positive patients are on antiretroviral therapy (ART). This has contributed to a significant increase in viral suppression rates and was achieved among 59% of patients in 2015.
According to the United Nations Sustainable Development Goals, the detection, treatment, and immune suppression rates should all be 90%. According to the aforementioned data, Georgia does not meet these criteria (51%, 70% and 59%, respectively).
The number of detected TB cases has been decreasing over the past six years. Nevertheless, the prevalence of resistant and multidrug-resistant (MDR) TB remains a significant challenge (see Figure 3), as it increases the social and economic burden of the disease. Drug-resistant TB constitutes 12% of new TB cases, which is alarming. The success rate for treatment of MDR-TB is only 43%, and one in every three patients is lost to treatment and does not complete the course. Approximatly 89% of TB patients are aware of their HIV status. The success rate for treatment of drug-resistant TB and HIV co-infection is low at only 29%.
Although the Global Fund and other donors have been supporting HIV and TB interventions, Georgia faces a number of challenges. The expected termination of donor aid requires the country to ensure a smooth transition of the disease prevention and treatment programs to domestic sources. The TSP has been devised to serve this purpose.
The TSP was developed in 2016. This process was funded by the L. Sakvarelidze National Center for Disease Control and Public Health (NCDCPH), the Principal Recipient of the Global Fund grant. The TSP is based on the results of a Transition Preparedness Assessment (TPA) conducted in 2015 by the Curatio International Foundation (CIF) with the Global Fund’s financial support. CBOs and CSOs were actively involved in the TSP development process in the shape of the Policy and Advocacy Advisory Council, and the interim versions were also reviewed by the Country Coordinating Mechanism (CCM). The final version of the document was approved by the CCM in 2017.
Purpose of the TSP and funding prospects, other related documents, and processes
The transition period for funding national HIV and TB programs began in 2015. The transition period includes the gradual takeover of Global Fund and other donor-supported activities by the Government of Georgia.
The TSP includes only the activities in the transition period that are not included and budgeted for:
a) within the programs currently funded by the Global Fund and other donors; and
b) b) in the current and future National HIV/AIDS Strategic Plan for 2016–2018 and the National TB Strategic Plan for 2016–2020.
(Source: Interviews with individuals involved in the development of the TSP)
Consequently, the TSP does not provide a full picture of the transition process, unit costs, or sources of funding, and the aforementioned documents (national programs financed by the Global Fund, and the TB and HIV/AIDS Strategic Plans) should be reviewed jointly with the plan.
These two strategic documents (the TB and HIV/AIDS Strategic Plans) and the TSP jointly represent the country’s Action Plan for the transition period. The HIV/AIDS and TB strategies focus on the provision of disease management services, while the TSP focuses on strengthening health systems and improving governance and legislative environments.
It is noteworthy that all those strategic documents have a budget. However, to ensure that funds are actually allocated, this obligation should be reflected in the country’s Basic Data and Directions (BDD) document. The BDD defines the State’s budget priorities and the appropriation limit of budgetary allocations (i.e. the amount of funds that can be mobilized by the government). Besides the BDD, the budget of the current fiscal year is also an important document, as it includes specific details of the allocations. Finally, the document stipulating the national programs (in this case, these are the programs of the Ministry of Labour, Health, and Social Affairs of Georgia (MoLHSA), which would be approved by the Government of Georgia) provide actual details of the budget implementation, unit costs, total allocation per activity, procurement modalities, etc.
The combination of all these documents constitutes the basis for an unbiased assessment of the transition process.
According to the experts, it is essential to specify the activities of the Global Fund programs which will be extended to 2019–2020. This can be done in the process of developing the new HIV/AIDS and TB Strategic Plans for 2019–2023. Otherwise, there is a risk that it will be difficult to provide the Ministry of Finance with justification for the significant budget increase needed, and this may result in a lack of funding for different services — for example, preventive interventions, peer-driven services, etc. for KAPs (MWM, PWID, FSW)
This section summarizes the goals and activities of the TSP for each of the main blocks in which community and civil society engagement is crucial in the authors’ opinion. HIV and TB activities are distinguished from each other by color: HIV activities are shown in red, and TB activities in blue (in the online version, this is marked with the drop-down arrow). Activities related to both HIV and TB are marked in green.
The goal of the TSP is to ensure a smooth transition from Global Fund funding towards fully national funding of the national HIV and TB response by 2022:
The expected challenges can be overcome by actively engaging civil society in the processes of developing the aforementioned strategies, planning budgets, and monitoring program implementation
The TSP consists of several large documents.
First of all is the main body of the TSP, which includes information about: (1) the current situation; (2) challenges; and (3) tasks and activities planned to overcome these challenges.
The information in the TSP text is divided into blocks. The External Environment section includes: (1) political; and (2) economic blocks. The Internal Environment includes the aspects of program implementation and financial sustainability: (3) financial resources; (4) human resources; (5) infrastructure; (6) the health information system; (7) governance; (8) accountability; (9) service delivery; (10) procurement and supply management; (11) organizational capacity; and (12) transition planning.
In addition to the main document, the TSP includes the following appendices: (I) Timeframe of Activities and Responsibilities; (II) Monitoring and Evaluation Framework; and (III) Budget.
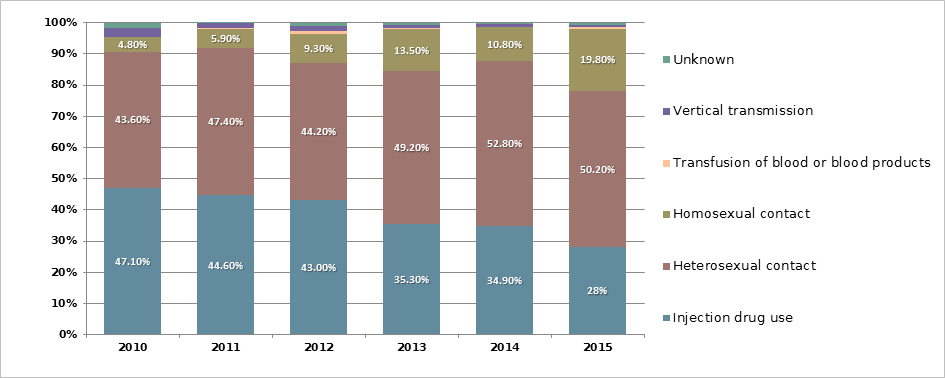
Figure 1. HIV prevalence by mode of transmission in 2010–2015, Source: NCDCPH
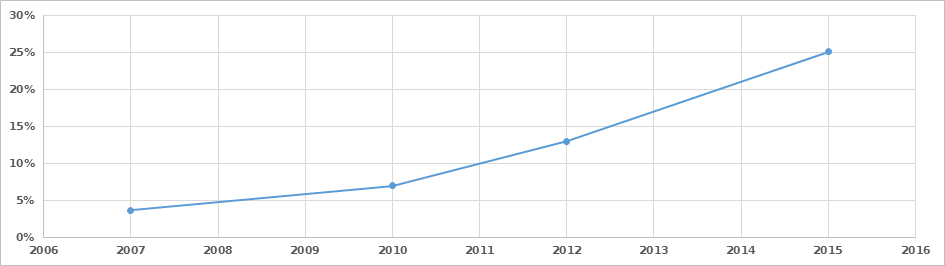
Figure 2. HIV prevalence among the MSM population, Tblisi, 2007–2015, Source: NCDCPH
Tuberculosis
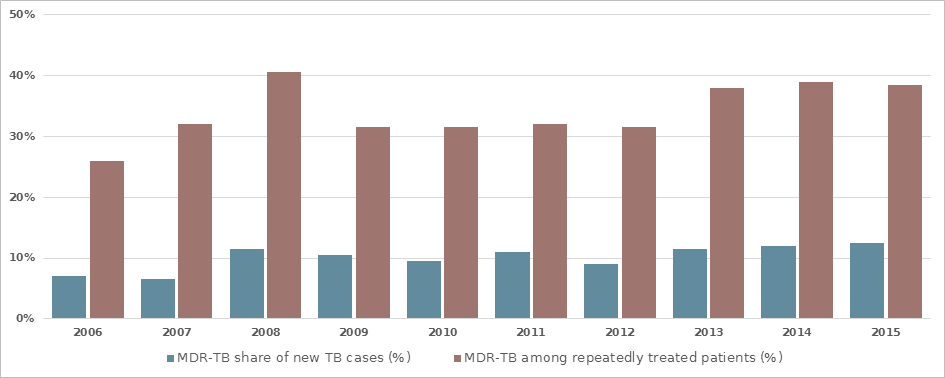
Figure 3. MDR-TB in Georgia, Source: NCDCPH; National Center of Tuberculosis and Lung Disease (NCTLD)
Important Facts about the Transition and Sustainability Plan
General Information about the Development of the Transition and Sustainability Plan
Brief Overview of the Transition and Sustainability Plan and an Analysis of the Current Challenges
TSP Structure and Appendices
| Objective 1.1.1. Create conducive legal environment for HIV national response | Objective 1.1.2. Create enabling environment for CSO engagement in HIV &TB national response | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 1.1.1.1. Increase Coordination among key players, relevant government bodies, Parliamentary committees, Civil Society, the National Platform on Drug Policy Reform to change drug legislation in the country. | Activity 1.1.2.1. Review State Procurement Law and relevant regulations to identify potential barriers for CSO-contracting to deliver HIV and TB community services under the state funding. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 1.1.1.2. Monitor and foster policy interventions to remove the legislative barriers to access to HIV Prevention and harm reduction service in civil and penitentiary sectors. | Activity 1.1.2.2. Assess the barriers and opportunities for CSOs to satisfy the state procurement requirements and in case of need – to develop and adopt detailed operational manual describing the rules and procedures for contracting CSOs for health service delivery. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 1.1.1.3. Support development and enforcement of the new Four-pillar Drug Policy, Anti-Drug Strategy and Action Plan. | Activity 1.1.2.3. Build Capacity for CSOs, their networks and coalitions – through training and technical assistance in management, resource mobilization for CSOs/CBOs to satisfy the state procurement requirements. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
All activities included in this block are highlighted, because this section is crucial to provide a favorable environment for the KAPs.
Activities 1.1.1.1 to 1.1.1.3 in the draft TSP (a version before the version approved in January 2017) included abolishing criminal prosecution for drug use — in particular, removing Article N273 from the Criminal Code of Georgia. The final document suggests revising the legislation and enforcing a four-pillar drug policy. Enforcement of the four-pillar drug policy should be regulated under the Strategy and Action Plan developed by the Anti-Drug Interagency Council. In 2014–2015 a similar drug policy was enforced, although observation of the law and practice suggests that it will be impossible to implement such a balanced policy unless there is shift from the current repressive approach to drug policy to a public heath-oriented one.
Such changes in the final version of the TSP suggest that Georgia is still not ready to give up repressive, punishment-based drug policies.
An indicator of the activities in this block is the process of working on the package of legislative changes with the participation of the Parliamentary Committee on Healthcare and Social Issues and the National Platform on Drug Policy Reform. Review of the law has not begun yet, and there is no guarantee that the punishment-based drug policy will change as a result of this process.
With regard to public procurement, there is currently no legal barrier (Activity 1.1.2.1.) to awarding contracts to CSOs, although the rigid tender procedures restrict the participation of financially/organizationally weak or not-for-profit entities (e.g. they are unable to submit the bank guarantee required under the terms of the tender).
To solve this problem at the legislative level, it is necessary to amend the State Procurement Law with regards to social contracts. This is less likely to happen. The TSP directly states that the intention is not to amend the State Procurement Law but to study barriers to civil society participation in public tenders and to enable this sector to submit bank guarantees. Local experts often offer an argument that the State Procurement Law of Georgia is highly acclaimed by international experts. However, even if the law is good, it does not mean that it cannot be improved. Civil society must make a joint effort to provide the Government of Georgia with a clear justification for the legislative changes to ensure that an amended law facilitates, rather than hinders, the CSOs’ activities.
Overcoming challenges requires more in-depth analysis of existing regulations and, on the basis of identified gaps/barriers, the adoption of a detailed operational manual describing the rules and procedures for CSO contracting for health service delivery with the participation of civil society and other stakeholders (Activity 1.1.2.2.). It is also important to build the capacities of CSOs to enable them to meet the state procurement requirements (Activity 1.1.2.3.). It is necessary to organize training to enable CSOs to manage programs and mobilize the necessary resources more flexibly when participating in public procurement processes. Civil society should be actively involved in the development of a training curriculum and in conducting training. However, this should be done against a background of government recognition of the unique role of these organizations by making the relevant amendments to the law.
| 2.1.1. Financial Resources – HIV | 2.1.2. Financial Resources – TB | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Objective 2.1.1. Ensure full budgetary commitment and allocative efficiency for national HIV response | Objective 2.1.2. Ensure adequate funding and allocative efficiency for the national TB response | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.1.1.1. Conduct HIV program allocative and technical efficiency study to inform HIV strategic planning during the transition period. | Activity 2.1.2.1. Fill the gaps in the financing of the National TB Program. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.1.1.2. Support the Government of Georgia to establish a System of Health Accounts that will regularly monitor HIV expenditure data and generate reports that are public accessible. | Activity 2.1.2.2. Ensure mobilization of funding for continuous education for TB personnel (funding sources for CPD courses). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.1.1.3. Provide capacity building and TA to relevant local staff to ensure that the SHA is functioning properly. | Activity 2.1.2.3. Conduct TB Spending data analysis on an annual basis. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.1.1.4. Conduct HIV/AIDS Spending data analysis on an annual basis. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.1.1.5. Allocate commensurate funding for prevention programs targeting KAPs including low threshold services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.1.1.6. Align state funds allocation to epidemiological priorities for each key population affected to ensure allocative efficiency. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.1.1.7. Ensure state funding to support HIV-related studies, including second-generation studies (Population Size Estimation studies, IBBSs among KAPs). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.1.1.8. Engage with relevant ministries (MoES, MoC, MoYS) and local governments, city mayors and municipalities to encourage their engagement in multi-sectoral HIV response. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The active involvement of CSOs and CBOs is one of the most sustainable ways to protect the interests of communities and ensure the sustainability of services in the state budget planning and monitoring process.
To this end, it is recommended to implement advocacy activities regularly and to monitor current funding and commitments undertaken under the TSP and other related documents (National Plans for HIV, Hepatitis C, and TB). To carry out regular monitoring, it is recommended to develop mechanisms that will ensure that CSOs are involved in this process. Reports on public spending on HIV/AIDS and TB services and outcomes should be submitted to the CCM and the Policy and Advocacy Advisory Council on an annual basis (Activity 2.1.1.2.). Moreover, the national accounts of HIV/AIDS and TB expenditure should become publicly available (on the MoLHSA website).
To ensure effective public/civil society oversight, CBOs and CSOs should create a unified matrix of public financial obligations, including financial obligations determined by the TSP and other related strategies and state-funded programs. Such an approach will enable the development of an effective mechanism to identify any duplicate commitments (i.e. obligations included in several plans) and to measure and monitor the total amount of state financial obligations.
The process of transition from Global Fund funding to national funding has already begun. However, there are a number of services that still fully depend on Global Fund funding. It is essential to ensure the sustainability of these services after the Global Fund’s aid is withdrawn.
It is important to ensure the direct involvement of more CSOs and KAPs in the budget planning process. This will improve the opportunity for public/civil oversight.
Mechanisms for involving the CCM and the Policy and Advocacy Advisory Council in the budget process for the national HIV/AIDS and TB response need to be developed.
According to the main body text for this activity, funds to support its implementation will be “allocated”, although the document’s Monitoring and Evaluation Framework says that funds should be “advocated for”.
According to the TSP, the new National Strategic Plan for HIV/AIDS will be based on a technical and allocative efficiency study (Activity 2.1.1.1.). Therefore, it is important to inform and actively involve CSOs and CBOs in this process, as the findings of this study will serve as the basis for costing and budgeting for low-threshold services.
The OPTIMA (Optimizing Investments in Georgia's HIV/AIDS National Response) (Activity 2.1.1.6.) suggests that the distribution of resources will be effective for targeting men who have sex with men and women (MSMW) due to the highest HIV prevalence in this group. It is noteworthy that despite the low HIV prevalence among PWID, they remain one of the priority target populations for the national HIV/AIDS response, as it is the largest group affected by HIV, and there is a significant risk for the rapid spread of HIV.
It is crucial to sustain funding to maintain and improve the outcomes achieved so far. The distribution of resources should not be based only on epidemiological data. For example, decreases in the level of funding for harm reduction activities in other countries have resulted in increased HIV prevalence among PWID. On the other hand, this approach is supported by the fact that due to the previously low HIV prevalence among MSM, services for them were not considered a priority, thus the amount of funds allocated was small; as a result, prevalence in this group has reached 25.1%. We welcome the efforts to focus on the needs of MSM, despite the significant delay. The government should understand that improvements cannot be achieved at the expense of reducing services for other groups.
After the completion of the Global Fund programs, the government should also allocate funds for HIV-related research (Activity 2.1.1.7.), including population-size estimation studies (IBBSs) that will facilitate the study of risk behavior among high-risk populations and tailor funding to needs. To ensure financial sustainability, it is recommended to include this activity in the new HIV/AIDS Strategic Plan for 2019–2023 and to define funding sources. It should be noted that these studies are very important
The TSP also addresses the diversification of budget resources. Due to the reduction in donor funding and fluctuations in currency exchange rates, the financial burden on the Ministry of Health is likely to increase significantly. Therefore, it is necessary to attract additional resources from other government agencies (e.g. the Ministry of Education and Science of Georgia, the Ministry of Sport and Youth Affairs of Georgia, the Ministry of Defense of Georgia, the Ministry of Corrections of Georgia, etc.), local governments, and city municipalities. It is important to encourage engagement of the private sector in the national HIV response (Activity 2.1.1.8.). The TSP states that civil society is responsible for budget advocacy at a local level (from local budgets), although the involvement of central government authorities in this process will have a significant impact, and CSOs/CBOs should try to initiate such cooperation.
Filling funding gaps in the national TB program (Activity 2.1.2.1.) is also an important activity that should be monitored by the public sector. For example, according to the Monitoring and Evaluation Framework, the level of state funding will increase from 46% in 2015 to 80% in 2021.
| 2.2.1. Human Resources – HIV | 2.2.2. Human Resources – TB | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Objective 2.2.1. Ensure adequate staffing in HIV response. | Objective 2.2.2.1. Scale-up and the nationwide implementation of the human resources plan and RBF mechanism for the integrated and patient-centred model of TB care. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.1.1. Develop policy for production and continuous professional development of human resources for HIV/AIDS programs, including CSO personnel (risk reduction and VCT consultants, outreach and social workers, peer-educators, treatment regimen support consultants). | Activity 2.2.2.1.1. Adopt, monitor and support the implementation of long-term master plan for the integrated model for TB services. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.1.2. Integrate HIV training modules in the formal education system at the undergraduate and postgraduate levels. | Activity 2.2.2.1.2. Support the scale up of Results-Based Financing (RBF) mechanism for nationwide implementation. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.1.3. Provide training of trainers, including that for academia staff on HIV-related topics. | Objective 2.2.2.2. Ensure production and continuous professional development of human resources for TB program, including policies for developing CSO | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.2.2.1. Develop policy for production (professional competencies/qualification framework, course accreditation, and certification) for non-medical staff/CSO personnel (e.g. outreach and social workers, case managers, peer-educators, treatment regimen support consultants, self-support group facilitators, community officers) as well as medical personnel of PHC. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.2.2.2. Ensure adequate allocation of public funding for Continuous Professional Development courses. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.2.2.3. Introduce free of charge residency courses for understaffed specialties, i.e. such as Pulmonology and Pthisiatry specialties. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.2.2.4. Ensure periodic updates for TB care guidelines. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.2.2.5. Support the institutionalization of TB training through integrating training modules into formal education system. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.2.2.6. Support the development of a network of master trainers for TB. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.2.3. Infrastructure - Health and non-Health equipment for HIV and TB programs | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Objective 2.2.3. Ensure adequate O&M for health and non-health equipment for HIV and TB | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.2.3.1. Provide O&M for health and non-health equipment. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
For the national HIV/AIDS response, staff training — in particular, for NGO staff — is crucial. The existing service model envisions the involvement of voluntary counseling and testing consultants, peer educators, outreach and social workers, and treatment adherence consultants, and most of the people employed in these positions have not received any formal education in service delivery. CSOs/CBOs must participate in training and in devising state regulations for these professions. This process should also ensure that community representatives are actively involved in service delivery.
The development of a professional competencies framework for non-medical staff in TB-related fields is planned, similar to that for HIV-related fields.
The applicable laws envisage a professional competencies framework for medical staff and certified social workers. Consequently, in the implementation process of the TSP, a similar system will be created, which may have a crucial impact on the employment prospects of existing employees (or new ones) to deliver community services.
In total, US$32,600 are allocated for the elaboration and approval of the policy on the professional development of human resources in HIV-related fields for 2018–2019 (Activity 2.2.1.1.). However, this amount is not intended for staff training (including NGO personnel); it is intended for the elaboration of a policy for the continuous professional development of human resources. It will be important to monitor the process of budgeting for staff training in accordance with this policy during the development of the National Strategic Plans.
It is essential to ensure the involvement of civil society in the adoption of the master plan for the integrated model for TB services and the integration of TB training into the formal education system (Activities 2.2.2.1.1, 2.2.2.2.1, and 2.2.2.2.5.). Today mainly universities and professional associations are meant to be involved in these activities.
| 2.3.1. Health Information System – HIV | 2.3.2. Health Information System – TB |
| Objective 2.3.1. Sustainable development of Health Information System in HIV national response | Objective 2.3.2. Improve the health information systems for TB |
| Activity 2.3.1.1. Monitor and evaluate (by the end of 2017) the HIS strengthening interventions and the process of full integration of advanced surveillance, monitoring and reporting system. | Activity 2.3.2.1. Monitor and evaluate (by the end of 2017) the process of full integration of advanced monitoring and reporting system (planned under new TB grant). |
| Activity 2.3.1.2. Plan and implement measures identified through the planned HIS evaluation to support the full institutionalization of the HIS for HIV national response (TBD). | Activity 2.3.2.2. Plan and implement measures identified through the planned HIS evaluation to support the full institutionalization of the HIS for TB national response (TBD). |
| Activity 2.3.2.3. Train TB staff in the information system's use. |
| 2.4.1. Governance – HIV Governance (Political support, Program Leadership, Coordination) | 2.4.2. Governance – TB | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Objective 2.4.1. Improve HIV program governance | Objective 2.4.2. Improve governance for TB national response | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.4.1.1. Develop costed HIV/AIDS National Strategy for 2019-2023 and Action Plan. | Activity 2.4.2.1. Ensure the codification of the roles and responsibilities for TB program implementation management through the adoption of legal document (Government of Georgia resolution and possible changes to the TB Law). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.4.1.2. Approve the HIV/AIDS National Strategy for 2019-2023 and Action Plan by the Government resolution. | Activity 2.4.2.2. Engage the relevant government agencies to explore and implement the regulatory mechanisms (e.g. licensing requirement) for private providers to retain the TB services beyond the mandated period (2018). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.4.1.3. Engage in dialogue with officials and key stakeholders to discuss recommended alternatives for positioning CCM adequately within the government hierarchy and implement most optimal option that will ensure sustainability of legally empowered CCM structure. | Activity 2.4.2.3. Develop costed TB National Strategy for 2021-2025 and Action Plan. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.4.2.4. Approve the TB National Strategy for 2021-2025 and Action Plan by the Government resolution to support its implementation. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The Governance block is crucial in defining the level of funding with which the country will completely replace the Global Fund and other donor funding. Even funding for low-threshold services (discussed under Block 2.6 below) will depend on the content of the National HIV/AIDS Strategic Plan for 2019–2023, its Action Plan (Activity 2.4.1.1.), and the budget.
The experts consider that the functions of the CCM (Activity 2.4.1.3.) should be maintained even after the completion of Global Fund programs. However, it is not explicitly guaranteed in the TSP, and it is less likely that the government will retain the CCM with its current composition (with a broader representation of civil society) and delegate to this body a right to define the demand for and supervise public budgets.
The participation of patient organizations, CBOs, or other CSOs in similar activities related to the TB response is similarly important (Activity 2.4.2.1. and Activity 2.4.2.3.).
| 2.5.1. Accountability – HIV | 2.5.2. Accountability – TB | ||||||||||||||||||||||||||||||||||||||||||||||||
| Objective 2.5.1. Improve HIV/AIDS program accountability to disseminate programmatic and financial data to key actors and wider public | Objective 2.5.2. Improving the National TB Program accountability to ensure that the information (programmatic and financial) is transparent and publicly accessible | ||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.5.1.1. Develop program outcome dissemination and communication strategy to ensure transparency and access to programmatic and financial data. | Activity 2.5.2.1. Regularly publish and make accessible the programmatic and financial reports on TB program implementation to all interested parties, including the CBOs and wider public. | ||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.5.1.2. Regularly publish and make accessible the programmatic and financial reports on HIV/AIDS program implementation to all interested parties, including the CSOs, beneficiaries and wider public. | |||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||
It is important to involve CBO/CSO activists and program beneficiaries in the activities in this block (Activities 2.5.1.1., 2.5.1.2, and 2.5.2.1) to ensure dissemination of information about outcomes in ways that are accessible and in a language understandable for all stakeholders. Monitoring activities in the information dissemination process (please see a detailed list) include the development of information dissemination strategies, which is also the responsibility of civil society.
| 2.6.1. Service Delivery – HIV | 2.6.2. Service Delivery – TB | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Objective 2.6.1. Improve HIV service delivery | Objective 2.6.2. Support the implementation of the Integrated, patient-centred care and prevention model | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.6.1.1. Advocate for approval and implementation of HIV prevention and harm reduction service national standards. | Activity 2.6.2.1. support the implementation and monitoring of long-term master plan for the integrated model for TB services. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.6.1.2. Train NGO staff to approve and support practical application of the national HIV prevention and harm reduction standards at various settings of service provisions. | Activity 2.6.2.2. Support the implementation of the quality improvement systems (implementation of evidence-based clinical practice guidelines, supportive supervision and performance review, quality measurement). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
National harm reduction standards were developed with the support of Eurasian Harm Reduction Network (EHRN) in 2016. The standards aim to improve the quality of harm reduction services. Service standards for HIV interventions targeting the MSM and commercial sex worker (CSW) populations are being developed with the financial support of UNFPA. According to recommendations based on OPTIMA findings, HIV prevention activities for MSM should include targeted services for MSMW (Activity 2.6.1.1.).
The service standards are a document that defines the volume of services and service delivery requirements (e.g. employees and their qualifications), and can be used to develop unit costs. Participation in the development, implementation, and further review of service standards is crucial for the community, as this document determines exactly how each person receives services when s/he applies to the service provider.
Standards should be approved to create a legal basis for service delivery. Moreover, they should be reviewed regularly.
According to Activity 2.6.1.2., 25–25 people will be trained in 2018–2019. It is noteworthy that this activity is not mentioned in the TSP Implementation Plan, although US$4,600 are budgeted for training each year.
| 2.7.1. Procurement and Supply Chain Management – HIV | 2.7.2. Procurement and Supply Chain Management – TB |
| Objective 2.7.1. Maintain the effective and functional procurement and supply chain for the HIV/AIDS health products by the relevant national structures | Objective 2.7.2. Maintain the effective and functional procurement and supply chain for the TB health products by the relevant national structures |
| Activity 2.7.1.1. Perform the procurement and supply chain assessment (by the end of 2017) for HIV/AIDS health products. | Activity 2.7.2.1. Perform the procurement and supply chain assessment (by the end of 2017) for TB health products. |
| Activity 2.7.1.2. Plan and implement capacity building for the national agency responsible for the procurement and supply (if a new entity will take over the procurement responsibility). | Activity 2.7.2.2. Plan and implement capacity building for the national agency responsible for the procurement and supply (if a new entity will take over the procurement responsibility). |
| 2.8.1. Organizational Capacity – HIV | 2.8.2. Organizational Capacity – TB |
| HIV national response is managed by the National Center of Disease Control and Public Health of the MoLHSA. The organization's capacity for program management, service delivery M&E, procurement and supply management is adequate creating enabling environment for the transition process. No specific activities are planned for these purposes. |
Objective 2.8.2. Strengthen the organizational capacity of the dedicated TB management agency (TBD under governance component) to improve coordination and management of national program |
| Activity 2.8.2.1. To implement capacity building activities in order to enhance the role of National TB Council (NTC) secretariat/the MoH Department of Health to provide operational and secretarial support to NTC as the coordination body for the national TB program. |
| Objective 2.9.1. Ensure that the TP is actionable and legally binding | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.9.1.1. Approve the TP with actionable indicators and milestones through the Government Resolution. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Activity 2.9.1.2. Establish external Peer Review Mechanism for monitoring the implementation of Transition Sustainability Plan as well as TGF grants and National Strategic Plans for HIV and TB to promote adherence to and fulfilment of declared commitments from the State as well as other programs. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
This block includes important measures for the transition process. Both activities should ensure flexible and uninterrupted transition of the national HIV and TB response. The obligatory nature of the plan and the need for systematic monitoring are underlined in the activities. Besides the TSP, CSOs and CBOs should consider the National Strategic Plans for HIV and TB and activities planned within the Global Fund programs with regard to monitoring.
The transition process from donor funding to domestic funding in the framework of the TSP and the national HIV/AIDS and TB response offers multiple opportunities for CSO and CBO engagement and most importantly, proves the necessity of this engagement.
Some important recommendations in this regard are as follows:
- The TSP is not a final plan for the transition process. Therefore, community and civil society activists’ engagement in the development of the National Strategic Plans for HIV and TB, the formulation of indicators and budgets for those plans, and participation in the development of state budgets and programs is crucial.
- CBOs and CSOs must continue to work to remove legislative barriers. Without clear targets and indicators, it will be impossible to provide services on the scale and in the way that would be necessary, for example, to achieve the United Nations Sustainable Development Goals.
- It is no less important to ensure that CSOs document barriers in the state procurement system in order to overcome those barriers, not by artificially fitting CSOs into the current system, but by protecting the interests of the wider public.
- To fill the funding gaps, budget advocacy work should start right now to ensure that public allocations are in place after the termination of Global Fund funding. Moreover, each of these gaps must become a target for joint advocacy by communities.
- The TSP suggests resource allocation by epidemiological indicators that would be acceptable to stop uncontrolled epidemics, but it must not be done at the expense of preventive programs, which have already produced results and show good coverage and efficiency outcomes (harm reduction activities). Otherwise, we will get a situation where the resources allocated are insufficient for either a rapid reversal of the epidemics in one group or for maintaining the epidemiological targets of another group.
- It is crucial to review the TSP and its performance indicators, and reinstate the formulations included in the previous draft version. According to the current formulations, the plan will be considered fulfilled if, for example, drug policy is tightened, since the indicator requires only change, but does not specify the direction. The government should understand that implementation of the TSP is inevitable, not as a counterweight to receiving the remaining funding from the Global Fund, but to ensure the well-being and health of its citizens.
| AIDS | Acquired Immune Deficiency Syndrome |
| CBO | Community-based Organization |
| CCM | Country Coordinating Mechanism |
| CSO | Civil Society Organization |
| FSW | Female Sex Worker |
| GARP | Global AIDS Response Progress |
| HIV | Human Immunodeficiency Virus |
| IBBSS | Integrated Bio-Behavioral Surveillance Survey |
| KAP | Key Affected Population |
| M&E | Monitoring and Evaluation |
| MDR | Multidrug-resistant |
| MoLHSA | Ministry of Labour, Health, and Social Affairs |
| MSM | Men who Have Sex with Men |
| MSMW | Men who Have Sex with Men and Women |
| NASA | National AIDS Spending Assessment |
| NCDCPH | National Center for Disease Control and Public Health |
| NGO | Non-Governmental Organization |
| OST | Opioid Substitution Therapy |
| PWID | People Who Inject Drugs |
| TB | Tuberculosis |
| TSP | Transition and Sustainability Plan |

